On Vaccine Escape
Dr Geert vanden Bossche is a Belgian veterinarian with a PhD in virology. He came to prominence in March 2021 with an open letter to "all authorities, scientists and experts around the world" in which he called for a stop to mass vaccination due to concerns that the programme will 'select' more virulent vaccine-resistant variants, in an analogy with the evolution of antibiotic resistance. There have been numerous takedowns already, eg here, here and here, and there is no danger of his proposals ever being adopted, but his influence is significant in what we might call 'contrarian' circles, so, to echo Zuckerkandl and Pauling in a different context, "some beating of dead horses may be ethical, when here and there they display unexpected twitches that look like life"[1].
The first thing to note is that a great many advocates for vanden Bossche are anti-vaxxers, although not all may self-describe as such. They appear only to read the first two words of "don't vaccinate in a pandemic due to selection of vaccine escape". If you are of the vaccine-sceptic persuasion, think these vaccines don't work, and yet you support the ideas of vanden Bossche, let me stop you right there: how does that work? How can something that doesn't have any effect on the virus discriminate among variants in that way? Imagine that the vaccines contained only distilled water. Would that select for 'distilled water escape'? Alternatively, to borrow the analogy, consider the effect on resistance of an antibiotic that doesn't work. At all. What are they resistant to?
Beyond this cognitive dissonance, a few thoughts spring immediately to mind:
- Why would vaccination select for escape mutants, but natural infection would not?
- Why does selection for vaccine escape imply an increase in virulence - disease severity?
- For an individual, given that the result of vaccine breakthrough is an infection, does having an infection instead make strategic sense?
- What of the effect of mass infection on the generation of immune escape mutants?
- What of the effect of mass infection on
- economic activity
- hospitalisation
- Long Covid
- death
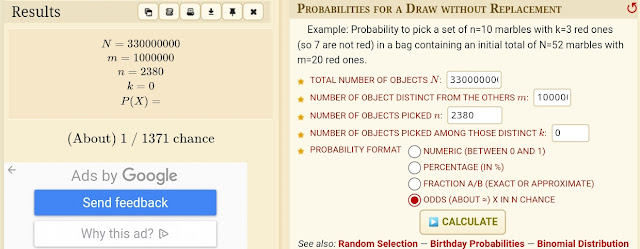
It can be useful to reduce to very simple models, and see what effect adjustment of the toy scenario to reflect more realistic assumptions might have. Consider two separate populations of a million individuals each. You have a 'leaky' vaccine which is 80% effective against transmission (through the combined risk reduction both of catching and of passing on the disease if caught). Unrealistically, assume no difference between the populations for
- per-case risk of hospitalisation (say 5%),
- death (1%),
- Long Covid (5%)
- Variants of Concern (1 per 200,000 infections).
Assume a R0 so high that the herd immunity threshold (1-(1/R0)) approaches 100%, and that immunity does not wane, ensuring a simple linear, density-independent relationship. Vaccinate everyone in Population B, no-one in A, and let the virus rip.
Population A (unvaccinated):
1 million infections
5 variants of concern
50,000 hospitalisations
50,000 Long Covid
10,000 deaths
Population B (vaccinated):
200,000 infections
1 variant of concern
10,000 hospitalisations
10,000 Long Covid
2,000 deaths
Population B (vaccinated; infection+severity):
1 variant of concern
5,000 hospitalisations
5,000 Long Covid
1,000 deaths
Mutation.
Natural Selection
Selective pressure can only have an effect on a population of replicators if it changes the relative performance of variants, compared to that in the absence of the pressure. For example if white bears have more offspring on average than brown ones in polar regions, then we would expect an increase in white and decrease in brown, in those regions. Elsewhere, the relative performance may be reversed: Selection is contextual.
Evolutionary biologists have devised the concept of 'fitness' to permit mathematical and computational treatments of selection. The fitness of a variant derives from the mean number of offspring accruing to its bearers. It functions as a mathematical exponent: a rate of increase or decrease. When two variants have different fitnesses, that with the greater will tend to displace the lower.
A similar measure is used to assess relative performance in epidemiology: the 'R value', a measure of the mean number of new infections per infection. If the native variant has a particular R value, and a novel variant arises with a greater R, the latter is expected to become dominant. This is observed with the delta variant of Covid. It is much more infectious - it has a higher R value than existing variants - and has rapidly become the dominant strain in many countries.
R can be influenced by both intrinsic and extrinsic factors. In the case of delta, the greater infectiousness is largely intrinsic: the viral sequence has mutations that increase infectiousness in all populations, the vaccinated and previously infected as well as the entirely non-immune. Vanden Bossche's concern incorporates an extrinsic factor - his anticipated Variant of Concern (VoC) preferentially evades vaccine-mediated immunity, but (somehow) not natural immunity to the same antigen. Therefore, by infecting more people than its rival, 'wild-type' strain, its R is proposed to be elevated in a highly vaccinated population. This same variant would tend to fizzle out in a population consisting solely of the infected and immunologically naive; it is increased by vaccination.
However, do these conditions ever exist? Why wouldn't infecting, in preference to vaccinating, have a similar selective effect, leaving us no better off?
Virulence
Note that the above selective considerations have little to do with virulence - the amount of
harm a particular variant causes in infection. There is a common but naive expectation that pathogens will evolve to reduced virulence in time, because it makes some sense to keep people circulating. Vanden Bossche's concern is the opposite - he insists vaccines will select for greater virulence. Neither of those is necessarily the case, because virulence and infectiousness are not always tightly coupled. Most of the adverse reactions in the sickest patients occur after the patient has finished shedding virus, so it gains no advantage either by keeping them healthier, or making them sicker.
Pathogens are simply selected to maximise R, ie to increase the number of additional infections per case, by whatever means. A particular mutation may cause virulence to increase, decrease or stay the same. It, or a different one, may cause R to increase, decrease or stay the same. There is no necessary relationship between the direction of these two parameters. All permutations are possible. If uncoupled from fitness (changes in R), virulence change thus becomes a dice roll, with more throws in an unvaccinated population.
In some circumstances (eg Marek's disease in chickens), increased virulence has been selected for; in others (eg Myxomatosis in rabbits) selection has favoured a reduction in virulence. It needs to be established, with much more rigour, whether the expectation here is increase, decrease or no change. Simply because Marek's (spread in crowded quarters through dust) has increased its virulence does not mean a respiratory virus of humans will. Marek's is a real problem, and we wouldn't wish to emulate the situation in poultry - the new variants are generally fatal to unvaccinated birds - but we would need to be very careful about leaping to a conclusion, in view of the considerable costs of not vaccinating.
What can be said with more certainty is that more virulent strains are more likely if there are more infections - ie, once again, we should reduce opportunities for mutation by maximal vaccination.
Models
Something noticeably lacking in vanden Bossche's argument is any attempt at quantification. Both evolutionary theory and epidemiology are fields with a significant mathematical and computational component. Presenting such models can give a useful cross-check on assumptions implicit in textual arguments. The strength of selection caused by vaccination must vary according to the number of individuals vaccinated, and the efficacy of the vaccine. A few vaccinated individuals, or a virtually ineffective vaccine, will exert virtually no selective pressure. Higher levels of efficacy and coverage, on the other hand, would presumably impart a significant advantage to an escapee. Yet at high levels, we would see a significant suppressive contribution from herd immunity, and a reduction of mutation. Therefore, it would be useful to get a handle on the shape of the graph of coverage vs strength of selection. Does vaccination start to exert significant pressure at low levels, or is the effect mostly confined to the upper portion? The virus experiences a trade-off. When vaccine takeup is low, replication is maximal, selection for escape is minimal. As more people get vaccinated or infected, the selective advantage becomes stronger, but at the same time the life is squeezed out of the virus by growing herd immunity. This complex dynamic has not been explored by vanden Bossche.
Here is an attempt to build such a model. It rapidly becomes densely mathematical, and bearing in mind that "all models are wrong but some are useful", the authors note:
The results from this model illustrate two insights: (i) vaccination aimed at reducing prevalence could be more effective at reducing disease than directly vaccinating the vulnerable; (ii) the highest risk for vaccine escape can occur at intermediate levels of vaccination.
This result is at odds with the textual model of vanden Bossche: target vaccination (if you have the luxury of choice, or are constrained) at reducing spread over protecting the vulnerable, and vaccinate as many people as possible. ie, aim for the situation in "Population B" above.
'Natural' vs vaccine immunity.
Vanden Bossche claims - without evidence - that vaccination somehow
interferes antagonistically with the innate immune response. But setting that aside,
which is better: infection-acquired or vaccine-stimulated immunity? That is, after all, the choice being presented; you have to do one or the other.
They are both natural, of course; both rely on the same immune system for their effect. The difference lies in the presentation of targets for the system to recognise, and the need for a little trickery to persuade the system to spring into action in vaccination. There are two stages to the immune response. Firstly, the innate system coarsely attacks the invader. Triggering of the innate system is followed by a cascade of responses that ultimately result in target-specific antibodies and 'memory' cells that can ramp up production of these antibodies on demand.
The SARS-CoV-2 genome is some 30,000 bases in length, generating about 29 proteins in total. However, only 4 of these proteins are present in an intact virion (virus particle), so until the virus enters a cell and its genome is translated, antibody targets are limited, and the deeper they are inside the virus, the less visible to antibody binding they are.
Antibodies
cannot 'see inside' intact viruses, so you need to attack something on the surface. Vaccines nearly all target the
spike (S), which gives coronaviruses their 'crown' appearance, and is the 'key' by which the virus unlocks the gateway to cells. Hitting this means that they cannot get into cells in the first place. Antibody attachment tags particles for attack by the immune system, but also interferes with binding of key to lock, helping to keep them out of cells.
Vaccine escape is also natural immune escape.
Vaccine escape is not impossible, but is rather rare. Marek's is the type case, but we aren't chickens, and SARS-CoV-2 is not MDV. It is a legitimate concern; we would be stuffed if we ended up with the situation in which we had to be vaccinated, as is the case for many factory-farmed chickens. However, given the prevalence of Covid, we can represent this as a straight choice - get vaccinated or get infected. Why would we get escape from vaccine-mediated immunity, but not infection? As a general rule, what is true for vaccine is precisely as true for 'natural immunity'. In this instance, given an equivalent efficacy and proportion of population immune, we would expect exactly as strong a selection pressure in the infected population as the vaccinated - with the addition of a higher rate of production of VoCs, due to the higher infection load.
It is tempting - a temptation to which vanden Bossche succumbs - to analogise vaccination with antibiotic use. However, in the antibiotic case the entire pathogen genome is available for mutation to potentially evade the threat. Antibiotics only work on bacteria, fully self-contained organisms. Bacterial genomes are about 150-200 times the size of a SARS-CoV-2 genome. They have their own metabolism, and thus a whole host of potential means by which an antibiotic might be dealt with by mutation. Viruses have much less latitude. The shape and charge pattern of the spike protein is constrained by the need to bind to angiotensin-converting enzyme, ACE2. It is a large protein, of rather static construction in evolutionary terms given our 20-year generation time. Although there are mutations in variants that have improved binding to ACE2, and others that have reduced antibody binding, there is a two-way constraint on the latitude for change. Weaken binding of antibodies, you may weaken ACE2 binding.
The spike is encoded by 3822 bases out of 30,000, or 12.7% of the viral genome. Mutations to the rest will be absolutely invisible to the vaccine; there is no mechanism that would allow vaccine escape by means of mutations taking place anywhere else in the genome. This doesn't eliminate escape, of course, but in combination with the mutational constraint just discussed it does reduce the size of the target, and hence the number of mutations that can hit it.
Additionally, the spike is quite a bit larger than a typical antibody. Many parts of its surface provide potential targets. Up to some 50 different 'epitopes', or antibody binding sites, are targeted. Mutation may weaken binding to one; it is very unlikely to do so to all. And if it does - to labour the point - this will affect 'natural' S antibodies to the same degree.
Where are they?
I was prompted to write this by the drumbeat conviction on social media that the sundry variants that have been thrown up are vindication of vanden Bossche's views. But in fact, all the variants so far have come from low-vaccination, or pre-vaccination, populations. Alpha, beta, gamma, delta, omicron ... they are all testament to the role of unrestrained replication in the generation of variants, not vaccination. They do, it is true, show signs of immune escape, but this is true of both vaccine- and infection-mediated immunity. There are no variants that evade vaccine but not infection, and none so far that show an increase in virulence - disease severity.
Omicron is the closest to a VoC arising in a vaccinated population, but South Africa presently has a vaccination rate of 24%. While omicron was cooking, that rate would have been less. It seems implausible that the causing of additional breakthrough infections in that 24% would provide a particularly strong selective pressure within the population as a whole. Far more important for evolutionary pressure are the infection of the fully susceptible, or the previously infected. Against those pressures, breakthrough in the 24% vaccinated must come a distant 3rd.
Postscript
[1] Evolutionary Divergence and Convergence in Proteins in Evolving Genes and Proteins, 1965, Bryson & Vogel eds


Comments
Post a Comment